Acute Sinusitis (Acute Rhinosinusitis): Classification, Clinical Manifestations, Diagnosis, and Treatment
A detailed review of rhinosinusitis, including classification, symptoms, diagnostic approaches, and current treatment strategies.
This article is for informational purposes only
The content on this website, including text, graphics, and other materials, is provided for informational purposes only. It is not intended as advice or guidance. Regarding your specific medical condition or treatment, please consult your healthcare provider.
Dermatological disorders of the external ear accompanied by pruritus — collectively referred to as pruritic dermatoses — comprise a group of inflammatory skin conditions affecting the auricle and external auditory canal, with intense itching as the primary symptom. These disorders significantly impair patient’s quality of life and require a comprehensive treatment approach, as they often reflect underlying systemic dysfunction.
In clinical practice, the following forms of pruritic dermatoses of the external ear are recognized:
The causes of auricular and external auditory canal eczema are multifactorial. Typically, the underlying trigger is a systemic condition, such as:
These, in turn, can often coexist with various ear disorders (such as recurrent chronic suppurative otitis media or intermittent skin trauma), which can exacerbate the pathological process.
Skin irritants play a key role in the development of contact (allergic) dermatitis, including:
Eczema is a long-lasting, relapsing, cyclical skin disorder. It arises from immunologic dysfunction.
The chronic phase is characterized by dry, flaky skin and lichenification (i.e., thickened and leathery skin). Additionally, the ear canal may become blocked by keratinized epidermis.
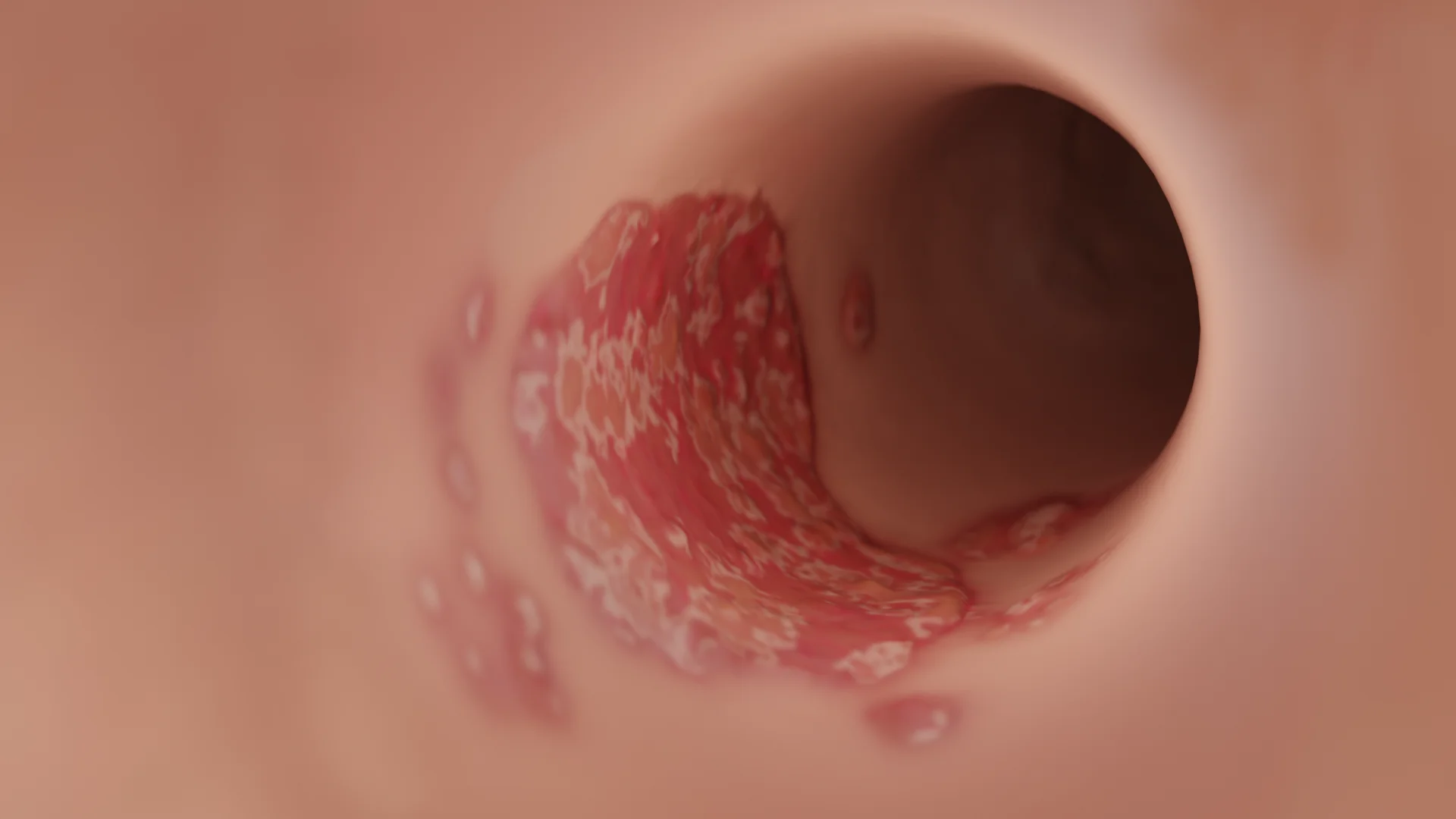
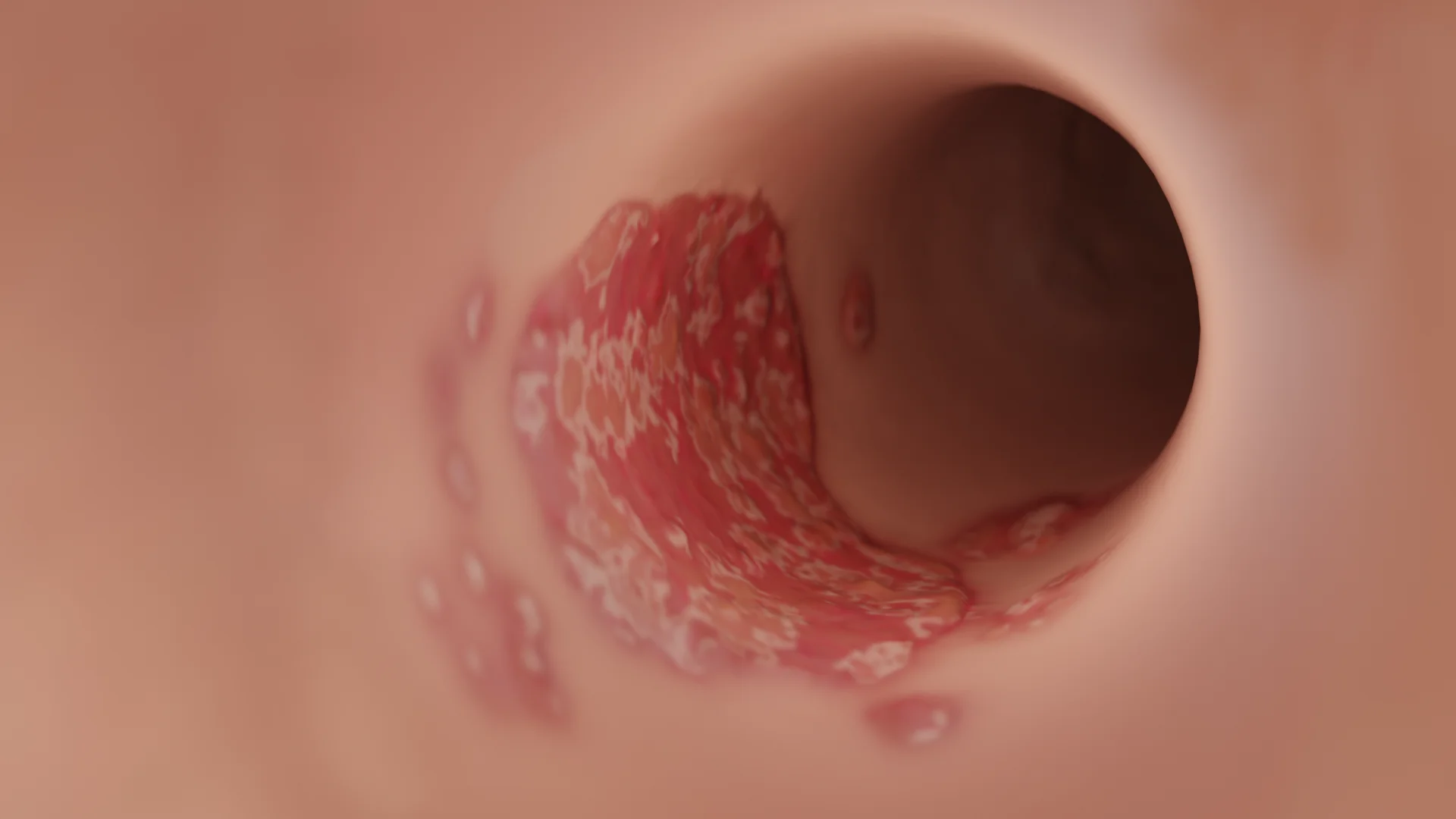
In the acute phase, vesicular rash secondary to hyperemia may develop. Vesicles tend to rupture and ooze serous fluid, leading to weeping. Subsequently, a crust forms over the lesions. Areas affected by eczema, which are exacerbated by scratching, can become infected. In this case, vesicles evolve into pustules that can also rupture and shed purulent fluid; the lesions are then covered by purulent crusts.
Allergic contact dermatitis is a delayed-type hypersensitivity reaction (type IV).
This condition involves pathological changes in the skin induced by either a prolonged sensitization or reexposure to an allergen.
Lesions that directly contact an allergen can develop vesicular rash and bullae filled with serous or hemorrhagic fluid. The skin is hyperemic and infiltrated. Ruptured vesicles and bullae contribute to crusting and scaling.
In the chronic phase, eczema of the auricle and the external auditory canal is identified solely by changes in skin appearance; other clinical manifestations are uncommon.
Symptoms of eczema in the acute phase:
Secondary infection can lead to purulent discharge, narrowing, and tenderness of the ear canal, which can hinder the diagnosis.
Note that eczema typically manifests with multiple lesions on the skin in the region of the radiocarpal joints, cubital fossae, face, and scalp.
Symptoms of allergic contact dermatitis:
Diagnosis is based on a patient’s medical history and physical examination.
General symptoms such as fever, chills, and signs of intoxication are rare, as well as deep auricular (ear cartilage) lesions and morphological changes.
Allergy testing may sometimes be utilized to diagnose the disorder and identify the underlying cause.
Differential diagnosis may be necessary when a secondary bacterial infection develops, in order to rule out acute otitis externa, perichondritis, acute suppurative otitis media, and other dermatitis types (including psoriasis and seborrhoea).
This category of disorders is typically subject to conservative treatment on an outpatient basis.
Contact dermatitis management can only be successful when the root cause is eliminated. Therefore, it is important to avoid any triggers, such as water contact and mechanical skin injuries, while the underlying extraorgan disease should be curtailed.
Please note that contact dermatitis management can only be successful when the root cause is eliminated. It is essential to prevent water exposure and mechanical trauma to the skin.
If a bacterial infection has developed, antibacterial ointments should be applied locally, any lesions should be regularly treated with antiseptic solutions.
Once the inflammation is under control, ointments containing glucocorticosteroids (GCS) and salicylic acid are typically recommended, with the latter having a keratolytic and regenerative effect. Oral antihistamines can help alleviate symptoms.
In the chronic phase, the skin should be regularly moisturized with liniments, while prolonged contact with water should be avoided. Physiotherapy, including UV exposure and ultra-high frequency (UHF) treatments, has been shown to contribute to positive outcomes.
1. What causes external ear eczema and contact dermatitis?
2. How do external ear dermatoses present, and what are the symptomatic differences?
3. When is differential diagnosis necessary?
4. How are external ear dermatoses treated?
5. What is the management strategy during eczema remission?
References
1.
VOKA Catalogue.
https://catalog.voka.io/
2.
Total Otolaryngology—Head and Neck Surgery, Anthony P. Sclafani, Robin A. Dyleski, Michael J. Pitman, Stimson P. Schantz. Thieme Medical Publishers, Inc., 2015. ISBN 978-1-60406-646-3.
3.
Бербом Х. Болезни уха, горла и носа / Ханс Бербом, Оливер Кашке, Тадеус Навка, Эндрю Свифт; пер. с англ. – 2-е изд. – М. : МЕДпреcс-информ, 2016. – 776 с. : ил. ISBN 978-5-00030- 322-1.
4.
Wilkinson EP, Fayad JN. Allergic Contact Dermatitis of the Auricle. Ear, Nose & Throat Journal. 2007;86(5):260. doi:10.1177/014556130708600502.
5.
Sood A, Taylor JS. Allergic contact dermatitis from hearing aid materials. Dermatitis. 2004 Mar;15(1):48-50. doi: 10.2310/6620.2004.20441. PMID: 15573649.
Summarize article with AI
Choose your preferable AI assistant:
Link successfully copied to clipboard
Thank you!
Your message is sent!
Our experts will contact you shortly. If you have any additional questions, please contact us at info@voka.io